ORIGINAL ARTICLES
Morbidity in children of less than one year of age in risky conditions: a prospective study
Mayckel da Silva Barreto1, Regina Lúcia Dalla Torre Silva2, Sonia Silva Marcon2
1Foundation of the College of Philosophy, Sciences and Literature of Mandaguari
2Maringa State University
ABSTRACT
Aim: To analyze the profile of morbidity of children in risky conditions during their first year. Method: This is a prospective study of a cohort type, performed in the municipality of Maringá, Brazil, over 12 months, with regard to 237 children in risky conditions, born between May 1st and October 31st 2008. Results: In the first year, 118 children (49.8%) needed at least one period of hospitalization. The majority were male (55%), within the first 15 days of life (72%), and underweight and premature (34.1%). Discussion: It was evidenced that, with the growth and development of the children, the reasons for hospitalization are switched from typical conditions of newborns in risky conditions to common illnesses of infancy. Conclusion: The findings confirm the necessity for a differentiated follow by the health team for children in risky conditions, in order to reduce the likelihood of hospitalization during the first year of life.
Keywords: Infant, Newborn; Morbidity; Hospitalization; Risk Factors.
INTRODUCTION
The presence of indicators regarding biological factors (history of hereditary diseases), behavioral (use of alcohol and illicit drugs) and sociocultural (low educational level with regard to mothers and teenage pregnancy), as well as the obstetric records(1), can be determining factors that can place a newborn (NB) in a condition of risk.
The birth and the follow up of children at risk is one of the contemporary challenges of healthcare service centers, as technological development and higher quality healthcare service has allowed the increasing survival of children born in unfavorable conditions. However, in spite of all the development that has added to the care of the newborn, they still have higher chances of falling ill and dying just after being born, and throughout the first year of lives, because of problems during pregnancy or labor(1).
Among the factors that can enhance the chances of a child at risk being hospitalized during his first year of life, we highlight being a male, having low socioeconomic status, living with a relatively high number of children under five years of age under the same roof, living in the urban area of a city, exposure to tobacco smoke, low temperatures and humidity, malnutrition, early ablactating, young mothers, low education of the mother, and high family density. Other risk factors associated with the health conditions of the child at birth are, for example, low birth weight and a low Apgar index (2-4).
The information regarding indexes and causes of hospitalization are important quality standards in terms of the offered service and, at the same time, are indirect indexes for the resolution of primary care. In terms of this view, the profile survey of morbidity of children under the age of one at risk is fundamental, because it is a basic parameter to measure the health needs of this segment of the population. Furthermore, it is directly related to determining factors that are beyond biological needs, including environmental conditions, nutrition, social, economic and cultural spheres, into which the children and their families are inserted(5).
The use of hospitalization, besides generating a significant degree of suffering for the family, is a costly event and can frequently be prevented by the use of primary care. For such preventive action, morbidity studies are of considerable relevance as they help to control diseases and to plan healthcare actions in both children’s hospitals and clinics. Normally these studies evaluate the severity of the incidence of diseases in children(6). Based on that, the aim of this study is to analyze the morbidity profile of children in risky conditions from birth to their first year.
METHOD
This is a prospective study, using a cohort approach, performed with children resident in the municipality of Maringá, Brazil, born between May 1st and October 31st 2008, and included in Maringá’s Newborn at Risk Vigilance Program.
This program was implemented in the city in 2000, with an objective to follow up all NB considered to be at risk, based on the following standards: low weight at birth (<2500g), Apgar score ≤ 7 at the 5th minute of life, gestation ≤ 36 weeks, maternal age ≤ 17 years old, congenital anomalies, mother diagnosed with HIV, low socioeconomic conditions and/or drug use by the mother.
The inclusion of a NB in this program is done by the epidemiology vigilance team of the municipality, which visits all hospitals, daily, to collect information with regard to born alive babies and to encourage the fulfillment of the necessary forms from the System of Information of Born Alive Children (SINASC, in Portuguese). When there is a birth that fitted into one or more of the criteria of risk conditions mentioned previously, the baby is included in the program while still hospitalized.
This inclusion is performed by the filling in of the admission form in two ways, and by an orientation meeting with the mother about the importance of the child’s medical follow up at a Basic Health Unit (UBS, in Portuguese), or by a private doctor. One of the copies of the admission form is sent to the UBS near to where the child lives and the other is filed at the Epidemiologic Vigilance Sector, based on the month of birth of the child.
The inclusion of the children in this study was done based on the forms filed every month, and using the same inclusion criteria as used by the Risky NB Vigilance Program. The criteria of exclusion were: families residing in other cities (21 cases – 5.4%); change of address without notification (51 cases – 14.6%); nonexistent address (11 cases – 2.8%) and; death of the child (18 cases – 4.4%). The follow up of NB was carried out over a period of 12 months, with visits at 15 and 45 days, and at the 3rd, 6th, 9th and 12th months.
The visits ended in October 2009, when the last children involved in this research turned one year. In the majority of the cases, the respondents were the mothers. In all meetings, the data was collected through an interview, using a semi-structured questionnaire, and involved a physical examination of the child, when anthropometrical data was obtained, as well as primitive reflexes and psychomotor development.
Morbidity in the first year was identified from reports during the visits and considered as such in the cases that hospitalization was necessary for a period of (or greater than) 24 hours, including during labor.
The quantitative information was stored in spreadsheets. The tables, processing and analysis of data was done using Excel for Windows® 2007. To present the results, we used tables of absolute and relative frequency. To verify the association of the studied variables with the outcome of interest we used statistical analysis through a chi-square non-parametric Pearson test, at a level of significance of p<0.05. The Odds Ratio (OR) was calculated to demonstrate the level of association of the variable with the hospitalization of the child.
This study followed the directives established by Resolution 196/96 of the Brazilian National Health Council. In addition, the research project was approved by the Permanent Committee of Ethics in Research with Human Beings of Maringá State University (Protocol 451/2008). The request to participate in the study was done personally to the mothers. At that time, they were informed about the research aims, the desire that they participate, the number of visits scheduled, the possible duration of each meeting, and the option to participate or not without any harm to the healthcare service to be provided to the children. After clarifying any doubts, the mothers that agreed to participate in this study signed a Free and Clear Consent Agreement (TCLE, in Portuguese) in two ways.
RESULTS
In the period between May 1st and October 31st 2008, 384 children were included in the Risky NB Vigilance Program of the municipality of Maringá. Of these, 237 were included in this research, because, besides those excluded based on the criteria used in this study, there were 42 families (10.9%) that refused to participate in this enquiry.
Of the 237 children included in this study, 118 (49.8%) needed at least one hospitalization in the first year, the majority of those involved being males (n=65 cases, 55%) and during the first 15 days of life (n=85 cases, 72%).
For the hospitalized children, their inclusion in the Risky NB Vigilance Program was done by the association of two or more criteria (n=34, 28.8%), followed by the age of the mother at 17 years or less (n=27, 22.9%), a gestational age equal to or less than 36 weeks (n=24, 20.4%), low weight at birth (n=16, 13.5%), and the presence of congenital anomalies and with an Apgar score equal to or less than seven at the fifth minute of life (n=08, 6.8% each) (see Table 1). However, the only risk factor associated with hospitalization was having a gestational age equal to or less than 36 weeks, as premature NBs had 2.5 times more chance of being hospitalized again when compared to other NBs at risk.
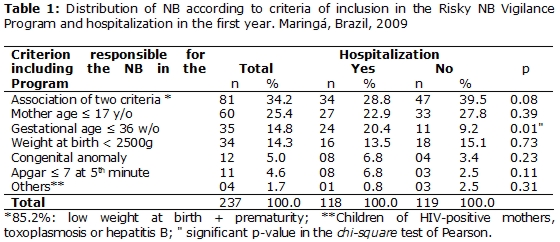
In a more specific format, it is observed that a meaningful number of the children hospitalized had two or more factors that placed them in a risky condition. From the total number of children monitored, 81 of them had two or more risk factors, and the concomitance of low weight at birth and prematurity constituted the most frequent associations that led to a scenario of risk (n=69, 85.2%).
The risk factor “mother age” equal to or less than 17 years of age were responsible for including 60 (25.4%) children in the Risky NB Vigilance Program, and from those, almost half (n=27, 45%) needed to be hospitalized during their first year of life. This was the most prevailing isolated risk factor among the hospitalized NBs.
In Table 2, we can observe that low weight at birth, associated with prematurity, was the most prevailing risk factor among the hospitalized NBs. Perinatal disorders, among them, the meconium aspiration syndrome and the neonatal icterus, make up the most frequent causes of hospitalization in this period, with 57 cases (67.1%), followed by respiratory issues with 11 cases (12.9%). The period of hospitalization varied from one to 90 days, averaging 12.4 days. Added to the last information, according to this study, premature NB present longer hospitalization periods.
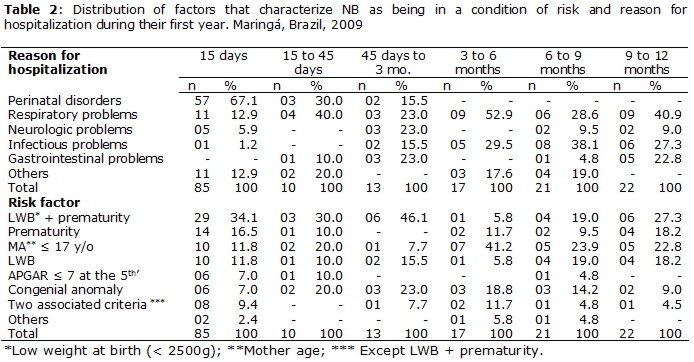
Between 15 and 45 days of life there was a considerable reduction in the number of individuals hospitalized, without a clear distinction among the sexes. The most significant risk factors of the children that were hospitalized were low weight at birth associated with prematurity (30%); congenital anomaly (20%), and the mother’s age being equal to or less than 17 years (20%). The main causes of hospitalization of this group were respiratory problems (40%) and perinatal disorders (30%). The period of hospitalization varied from one to 60 days, with an average of 12.7 days.
Of the 13 hospitalized children aged between 45 and 180 days, nine (69.2%) were female. The concomitant presence of risk factors such as low weight at birth and prematurity, was again the most prevailing risk factor found (n=06, 46.1%). The main causes of hospitalization were neurological, respiratory and gastrointestinal complications (n=03, 23% each). The average period of hospitalization was reduced to 10.8 days. However, one of the children was hospitalized for 90 days.
Between three and six months of age, from the 17 hospitalizations, nine (52.9%) were due to respiratory illnesses, especially upper respiratory tract infections (URTI) such as influenza, laryngitis and bronchitis. From the children hospitalized during this period, the risk factor “mother age equal to or less than 17 years old” was observed in seven (41.2%) cases. The period of hospitalization varied from one to five days, with an average of two days.
Between six to nine months of age, 21 hospitalizations were seen, of which eight (38.1%) were generated by infectious diseases. The risk factor “mother age equal to or less than 17 years old” were present in five cases (23.9%). The hospitalization period varied from one to 37 days, with an average of 5.8 days.
Between nine to 12 months of age, of the 22 hospitalizations that occurred in the studied population, nine (40.9%) were caused by respiratory diseases: five cases were diagnosed as pneumonia (55.5%), and the other four (44.5%) were URTIs. The infectious problems were the second most important cause of hospitalization, with six cases (27.3%). The gastrointestinal diseases were represented, in most of cases, by acute diarrhea, and were the third main cause of hospitalization (five cases, 22.8%). The average time of hospitalization was reduced to 2.6 days, varying from one to 15 days.
DISCUSSION
The hospitalization index observed in this study (49.8%) can be considered high, as it is almost three times higher than the same number found in the literature, which is partly due to the fact that the studied NBs are placed in conditions of risk. Consequently, they tend to be in a more fragile situation, thus leading to more hospitalizations. Such affirmation is corroborated by one study that compiled the results from two population surveys in the metropolitan region of São Paulo (Brazil), which found that the general proportion of the children hospitalized under one year of age (without observed risk conditions) rose from 7% in 1990 to 17% in 2002(7). Notwithstanding the rise observed in this period, the numbers are lower than those found in this investigation.
Regarding the factors that characterize the NBs as being at risk, we can highlight that low weight at birth associated with prematurity is the most frequent element mentioned. This happens because, in general, the pre-term labor generates the birth of a child without adequate body weight. This type of labor happens in 10% of the cases, depending on the studied population(4).
Prematurity and low weight at birth are determining factors of neonatal mortality, the development of infections and higher hospitalization rates, post-natal neuropsychological deficits and lower school performance, which can influence the health conditions of individuals throughout their adult life(4,8). Besides that, these children are more exposed to the risk of presenting inadequate immunological function, deficiency in terms of cognitive development, sudden infant death and a higher incidence of URTI(9).
According to what has been demonstrated in other studies, NB with low weight at birth are significantly more likely to be hospitalized, independent of the reason(4). It is believed that the reduction of NB with low weight at birth by the implementation of cost-effective strategies to monitor pregnant women, either in their regular pre-natal care consultations or in pregnant women’s support groups. This practice would significantly contribute to lowering the number of hospitalizations in the first year of the NBs.
An investigation performed in São Paulo which analyzed 368,980 declarations of live births of NBs, has 8.1% of individuals had low weight at birth(10). Another study, in the form of a literature review, demonstrated a 3.4% premature labor rate in the South of Brazil compared to 15% in the Southeast, between 1978 to 2004(11). More elevated rates were found in the study described in this paper, as only risky births were considered. However, it is important to highlight that local/regional differences influenced prematurity and low weight, and they must be considered in the planning of health programs and actions.
In terms of the hospitalized children of different ages below 12 months of age, it was seen that a significant proportion of them were of mothers who were 17 years old or younger. This finding underpins the need to maintain this criterion in risky NB vigilance programs in other cities of Brazil, because there is evidence that the babies of teenage mothers present higher biological risks such as prematurity, low weight at birth and respiratory problems, which will generate more hospitalizations in childhood(12).
A study performed in Londrina identified that 23.7% of NBs were included in the vigilance program of this municipality because of the mothers’ age being 17 years or less(13). In Sobral, almost 30% of the NBs with low weight were babies of teenage mothers(4). This same study showed that around 33% of the children that needed four or more emergency consultations during their first year of life were babies of mothers who were below twenty-four years of age(4).
This information reinforces the view that teenage pregnancy is a serious public health issue, because it represents risky conditions for the mother and the child. Thus, it is imperative that public health managers, the multiprofessional teams of the Family Health Strategy (ESF, in Portuguese) and the community in general, make efforts so that together they can introduce efficient interventions to diminish early pregnancy.
It is notorious that the children of teenage mothers fall ill, especially as a result of respiratory issues, possibly because the lack of experience when it comes to identifying and handling serious conditions. This situation of vulnerability must be considered during the follow up of risky NBs in primary care, by the clarification of possible doubts the teenage mother may have regarding dealing with the first signs and symptoms of a respiratory infection.
Another aggravator of the general health state of a NB is the Apgar score(1). For eight hospitalized children (6.8%) the criteria of inclusion in the program was severe hypoxia (an Apgar score equal or lower than seven at the fifth minute of life). This item must be considered by the healthcare team during the follow up of the child, as it is directly related to child morbimortality. A study performed in Recife regarding the risk factors associated with neonatal mortality of low weight NBs, found that severe hypoxia elevated the chances of death of the child by a factor of 44 (14). In addition, this last study also showed that the occurrence of severe hypoxia was the determinant factor with regard to low weight NB morbidity during the first year(4).
The presence of congenic anomaly was the basis of a risk criteria in terms of the other eight (6.8%) children that where hospitalized. The malformations, whenever present, developed into processes of morbidity that usually necessitated surgical proceedings and, in many cases, lead to the child’s death. The research performed in Recife showed that the presence of congenic malformation produced 5.6 more chances of the child dying during the first days of life because of illness complications(14).
As a whole, we can see that hospitalizations occur with a higher frequency (72%) during the first 15 days of life, and that the main causes were perinatal disorders – among them, meconium aspiration and neonatal jaundice – which together represented 67.1% of the reasons for hospitalization, followed by respiratory problems, found in 12.9% of the cases. The elevated number of hospitalizations in this period can be explained by the great number of children that, isolated or in association, were premature and presented low weight at birth. In fact, in the case of NBs, especially those at risk, the smaller they are, the more vulnerable they are to hospitalization(6).
According to what was identified in another study, the referral of pregnant women at risk to specialized units during the prenatal period and labor, and the presence of neonatal and pediatric Intensive Care Units (ICU), avoid the moving of both the mother during labor, and the premature baby, to a more complex hospitalization service in larger conurbations.
Hence, risky NBs could have survived using available technology found in local hospitals, which ratifies the seriousness of perinatal causes from hospitalization generating agents(7).
The great number of hospitalization cases due to infectious diseases that had started by the age of three months can be explained by the fact that, at that development stage, the child is particularly exposed to different environmental pathogens. It is also in this phase that new foods are introduced to the child’s diet, which explains, to a certain extent, the development of the first cases of severe diarrhea at six months in one of the children observed in this study.
However, with an improvement in the conditions on life of the population, and in the infrastructure of the cities, which will include better basic sanitation, we observe there is a reduction in hospitalizations because of illnesses due to a lack of sanitation. We can also include the vaccination program against rotavirus(15), included in 2006 in the Brazilian regular basic vaccination calendar, as another possible reason for the reduction in hospitalizations.
A study done in El Salvador demonstrated a reduction of 51% of hospitalizations of children with severe diarrhea after the implementation of vaccination against rotavirus(15). In the state of Paraná, where the vaccinations reached 80% of the population in 2008, a significant reduction of the coefficient of hospital morbidity by acute gastroenteritis for the children below one year of age(16) was observed, demonstrating that this public health policy has a positive impact on the morbimortality of the infant population.
At the end of the first year of life, respiratory diseases were responsible for more than 40% of the hospitalizations. Of these, 55.5% of the cases were diagnosed as pneumonia and 44.5% were identified as URTI. Brazil is one of the top 15 countries in terms of the high number of cases of pneumonia diagnosed in the infant population (below five years of age), with total of 1.8 million cases, with an estimated incidence rate of 0.11 episodes per child per year. In children below the age of five, more than 50% of the hospitalizations and 10 to 15% of the deaths were caused by acute respiratory infections (ARI), particularly pneumonia, responsible for 80% of the cases(17).
A study in São Paulo of children between zero and nine years demonstrated that the main reason for hospitalization was ARI, in particular pneumonia, with an ascending linear tendency in terms of the number of children affected by these pathologies, from 2002 to 2006(18).
The duration of hospitalization is directly related to the characteristics and the precedence of the patients, the ability to diagnose quickly, and the effectiveness of the treatment, as well as the efficiency of the supporting services that subsidize the recovery of the NBs (19). In this study, the average time of hospitalization reduced as the children at risk grew and matured. Notwithstanding this, the average stay in hospital - 12 days – can be considered elevated if compared to the Brazilian Health Ministry’s standards, which considers that children should be hospitalized for no longer than five days(20).
A Brazilian study identified, among 3,329 hospitalizations of children and teenagers that for those who were not in risky conditions, the average stay was three days(6). The research in Sobral, focused on low weight at birth NBs found that 61.5% of the hospitalizations happened during the prenatal period, with an average of 11 days(4). It is thus concluded that NBs with some risky conditions, are more vulnerable to hospitalization and those events tend to be longer than expected.
In a wider spectrum, it can be seen that, as the NB at risk grows and matures, the reasons for hospitalization are closer to those of the general infant population. As has been found in another piece of research(6), this period is characterized by a transition of typical disorders of NB at risk, such as meconium aspiration and neonatal jaundice, to health issues commonly found in infants, such as pneumopathies and infectious and diarrheal conditions.
According to the Brazilian Health Ministry, hospitalizations generated as a result of reasons that could be avoided by a significant primary healthcare presence, statistically included almost all infections of the upper and lower airways and gastroenteritis. It is hoped that this avoidable work does not develop to a point that would affect the access to, and performance of, the whole of the integrated health system(20) . The excessive number of reasons for hospitalization that could be avoided by a significant primary healthcare presence signals the need to analyze and resolve problems that would lead to a reduction in the number of hospitalizations. In addition, despite the fact that the NBs of this study are at risk, in terms of their greater susceptibility to illness, this same reason calls for the need for a differentiated follow-up with regard to this clientele, in order to reduce the potential damage to health, as well as to promote the child’s growth and development in a healthy manner.
CONCLUSION
The results of this study reaffirm that NBs considered to be at risk present a higher degree of fragility compared with regular NBs, as seen by the hospitalization rate during the first year of life, which was three times higher than the number found in the literature. In addition, we cannot disregard the fact that the hospitalization rate observed could be higher if all the children included in this investigation had been observed throughout the forecast period of 12 months.
The NBs that, over their first year of life needed most hospitalization, were those that had two or more criteria that would label them as being at risk, specifically the concomitance of prematurity and low weight at birth. Another important observation is that premature NBs had 2.5 more chances of being hospitalized during their first year than other NBs, which demonstrates the need for nursing staff to explore, together with the mothers, intervention strategies that minimize the occurrence of premature labor.
The criterion of inclusion that isolated one group from the others that caught the researchers’ eyes was mothers aged 17 years or less, ratifying this observation element as an important parameter that ought to be included in the Newborn at Risk Vigilance Programs. It is important to say that ESF must, through programs of education in health and the full observation of the population, clarify any doubts on the part of the teenage mothers, helping them to recognize signs of severe illnesses and the appropriate management of their children when facing adverse situations.
It was also seen that ARI was the main cause of hospitalization. Acute diarrhea cases were only present after the sixth month, as the number of infectious diseases rose after this period as a result of the introduction of new foods in the child’s diet and higher exposition to environmental pathogenics, respectively.
We believe that good coverage and quality in ambulatory care can reduce the hospitalization rate, and consequently, the subsequent deleterious effects on the child and the family. What is necessary is the constant monitoring of NBs at risk by the ESF team, especially because they present peculiar characteristics that make them more susceptible to illnesses in the first year of life. In addition, it is also necessary to develop research and local studies that deal with this topic, given that the characteristics of each place/region substantially influence the morbimontality of NBs at risk.
REFERENCES
1. Tamez RN, Silva MJP. Enfermagem na UTI Neonatal: Assistência ao Recém-nascido de Alto Risco. 4ª ed. Rio de Janeiro: Guanabara Koogan; 2009.
2. Macedo SEC, Menezes AMB, Albernaz E, Post P, Knorst M. Fatores de risco para internação por doença respiratória aguda em crianças até um ano de idade. Rev Saude Publica. 2007;41(3):351-58.
3. Oliveira EB, Melo ECP, Knupp VMAO. Perfil dos óbitos no município do Rio de Janeiro segundo peso ao nascer, no ano de 2002. Esc Anna Nery Rev Enferm. 2008;12(1):25-9.
4. Pinto JR. Morbidade de crianças com baixo peso ao nascer durante o primeiro ano de vida na cidade de Sobral, Ceará. Dissertação [ Mestrado em medicina ]. Universidade de São Paulo; 2010.
5. Santos PL. Morbidade referida, situação vacinal e acesso a serviços de saúde por pré-escolares. Medicina (Ribeirão Preto). 2009; 42(2):143-50.
6. Lenz MLM, Flores R, Pires NV, Stein AT. Hospitalizações entre crianças e adolescentes no território de abrangência de um serviço de Atenção Primária à saúde. Rev Bras Med Fam comunidade. 2008; 3 (12): 271-81.
7. Carvalho WO, Cesar CLG, Carandina L, Barros MBA, Alves MCGP, Goldbaum M. Inquéritos de saúde e uso de serviços materno-infantis em três municípios da grande São Paulo. Rev Panam Salud Publica. 2008; 24(5):314-23.
8. Autret F, Kieffer F, Tasseau A, Rigourd V, Valleur D, Voyer M, et al. Extreme prematurity: comparison of outcome at 5 years depending on gestational age below or above 26 weeks. Arch Pediatr. 2009; 16(7):976-83.
9. Gilbert NL; Fell DB; Joseph KS; Liu S; León JA; Sauve R. Temporal trends in sudden infant death syndrome in Canada from 1991 to 2005: contribution of changes in cause of death assignment practices and in maternal and infant characteristics. Paediatr Perinat Epidemiol. 2012; 26(2):124-30.
10. Minuci EG, Almeida MF. Diferenciais intra-urbanos de peso ao nascer no município de São Paulo. Rev Saude Publica. 2009; 43(2):256-66.
11. Silveira MF, Santos IS, Barros AJD, Matijasevich A, Barros FC, Victora CG. Increase in preterm births in Brazil: review of population-based studies. Rev Saude Publica. 2008; 42(5): 957-64.
12. Gallo PR, Leone C, Amigo H. Tendência de crescimento de filhos de mães Adolescentes. Rev. bras. crescimento desenvolv. hum. 2009;19 (2):297-305.
13. Rossetto EG, Pizzo LGP. Avaliação do programa de vigilância do recém-nascido de Londrina – Paraná. Cienc Cuid Saude. 2007; 6(2):148-56.
14. Ribeiro AM, Guimarães MJ, Lima MC, Sarinho SWk, Coutinho SB. Fatores de risco para mortalidade neonatal em crianças com baixo peso ao nascer. Rev Saude Publica. 2009; 43(2):246-55.
15. Palma O, Cruz L, Ramos H, Baires A, Villatoro N, Pastor D , et al. Effectiveness of rotavirus vaccination against childhood diarrhoea in El Salvador: case-control study. BMJ [ Internet ]. 2010 [ cited 2012 July 03 ] 14(340). Available from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2886195/
16. Rissardo LK, Furlan MCR, Marcon SS, Ferrer ALM, Oliveira RG. Hospital morbidity before and after vaccination program against rotavirus in the state of Paraná-Brazil: exploratory-descriptive study. Online Braz J Nurs [ Internet ]. 2010 [ cited 2012 July 03 ] ;9(2). Available from http://www.objnursing.uff.br/index.php/nursing/article/view/3053
17. Cardoso AM. A persistência das infecções respiratórias agudas como problema de Saúde Pública. Cad Saude Publica. 2010; 26(7):1270-71.
18. Ferrer APS, Sucupira ACSL, Grisi SJFE. Causes of hospitalization among children ages zero to nine years old in the city of São Paulo, Brazil. Clinics. 2010; 65(1): 35-44.
19. Ministério da Saúde [ BR ]. Secretaria de Vigilância em Saúde. Departamento de Análise de Situação em Saúde. Saúde Brasil 2007: uma análise da situação de saúde. Brasília: Ministério da Saúde, 2007.
20. Ministério da Saúde [ BR ]. Secretaria de Atenção à Saúde. Portaria nº 221, de 17 de Abril de 2008. Publica a Lista Brasileira de Internações por Condições Sensíveis à Atenção Primária. Diário Oficial da União 18 Apr 2008.
Received: 08/08/2012
Approved: 18/02/2013